Blog
Hypertrophic Cardiomyopathy is simply described as the hypertrophy of cardiac muscles, that is the abnormal stiffening and thickening of the heart muscles. Since it is categorized with the thickening of the heart muscles it leads to poor pumping of blood throughout the body that automatically leads to the shortage of oxygen transport in the body. Hypertrophic Cardiomyopathy is usually due to genetic variations that run in the family over the generation. It is called Familial Hypertrophic cardiomyopathy. On the other hand, hypertrophic cardiomyopathy is also observed in patients with no family history of HCM this condition is said to be non-familial hypertrophic Cardiomyopathy.
Facts to keep in mind
- Hypertrophic cardiomyopathy is associated with the thickening of left ventricle muscles, that is the main pumping chamber of the heart. Thus, it causes shortness of blood (oxygen) supply to the body.
- Hypertrophic Cardiomyopathy is often inherited, mutation in genes like MYH7, MYBPC3, TNNT2, and TNNI3 is found to be amongst the major causes of familial hypertrophic cardiomyopathy. Other genes may also be involved in this condition, including some that have not been identified.
- Familial hypertrophic cardiomyopathy is inherited in an autosomal dominant pattern thus even if one parent is defective for the gene it is transferred to the next generation. However, if the patient is homozygous for the mutation more severe symptoms have been reported.
- Non-familial Hypertrophic Cardiomyopathy is the result of tissue damage by heart attacks, long-term high blood pressure or metabolic disorders like diabetes or obesity.
- The symptoms for the disease vary widely from individual to individual and it usually goes unnoticed.
- Amongst the two categories it has been observed that familial hypertrophic cardiomyopathy affects every 1-in-200 people around the globe on an estimate, and it also accounts for more than 50% of all cases of Hypertrophic cardiomyopathy.
- Besides these categories HCM could either be Obstructive HCM (blocks blood pumping) or Non-Obstructive HCM (does not affect blood pumping or supply)
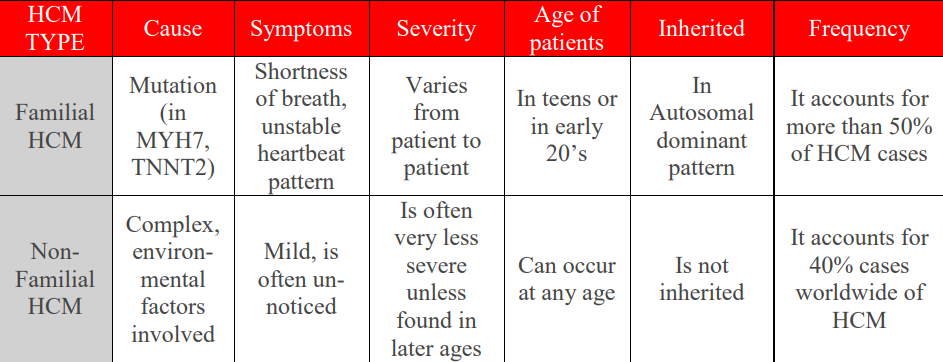 Fig-HCM1. Familial Hypertrophic Cardiomyopathy and Non-Familial
Hypertrophic Cardiomyopathy
Fig-HCM1. Familial Hypertrophic Cardiomyopathy and Non-Familial
Hypertrophic Cardiomyopathy
Causes and Effects of HCM
Familial Hypertrophic Cardiomyopathy:
As it is a genetic disease it is caused by mutation in either of the genes stated as:
- MYH7
- MYBPC3
- TNNT2
- TNNI3
It is to be considered that there are only 6 known and most observed genes whose mutation leads to HCM. Other causes or mutations are still unknown to researchers. To understand the cause completely one must understand that the protein products of these genes are the main players here as they play the most significant role in tensing of myocardial muscles by forming sarcomeres. The regular contraction and relaxation of these sarcomeres is the reason for the heart’s pumping. The gene MYH7 codes for a protein called cardiac beta (β)-myosin heavy chain that is the major component of the thick filament in sarcomeres. The gene MYBPC3 codes for protein named as cardiac myosin binding protein C. It is associated with thick filament and provides structural support and helps to regulate muscle contractions. The TNNT2 and TNNI3 genes provide information for making cardiac troponin T and cardiac troponin I, respectively. These are two of the three proteins required to make up the troponin protein complex found in cardiac muscle cells. The complex formed through these helps in regulating the contraction and relaxation of sarcomeres. It is still unknown how variation in these genes leads to hypertrophy and causes problems with the heartbeat. The mutants may result in formation of a changed sarcomere protein or reduce the protein's amount. An abnormality in any one of these proteins may affect the function of the sarcomere, disrupting normal cardiac muscle contraction. Research has also revealed that in HCM patients' contraction and relaxation of the heart muscle are abnormal, even before hypertrophy develops. However, it is not clear how these contraction problems are related to hypertrophy.
Non-Familial Hypertrophic Cardiomyopathy:
It is not a genetic disease thus its cause cannot be easily determined by tracing back the family history if variants of gene-products. Thus, researchers categorize its cause to be a complex procedure that involves the participation of genetic and environmental factors. HCM can affect the mitral valve of heart, the ventricular hypertrophy results in a dynamic pressure gradient across the left ventricular outflow tract, which further narrows during the systole. During systolic cycle, the mitral valve is pulled towards the sputum by mechanism like contraction of papillary muscle, however, the abnormality in the outflow tract and low pressure that occurs as blood is ejected at high velocity through the LVOT causes Ventrical Effect.
Symptoms
The symptoms of HCM are not very severe in earlier stages that often results in the disease going un-noticed. However, the common noticed and experienced symptoms amongst the patient are:
- Light-headedness
- Arrhythmia
- Chest pain (during tough activities)
- Fatigue
- Swelling in legs, feet
- Heart murmur
- Fainting
- Shortness of breath (usually during heavy exercises)
- Pounding feeling in chest
The effect of these symptoms varies highly from patient to patient, even in the family members having same or alike variations the symptoms can vary largely. However, it is observed that the symptoms are more severe in the patients who are homozygous for the condition.
Epidemiology of HCM
All around the globe the prevalence for HCM in general population is 0.2%, 1 in 500 people is suffering from HCM, that is determined by echocardiography. It is observed that almost 25% morphological evidence for HCM is found in the first-degree relatives. Furthermore, over the years it has been observed that men are more likely to be affected by HCM as compared to women. Since the mutation is autosomal dominant genetic inheritance for it most likely does not follow sex prediction.
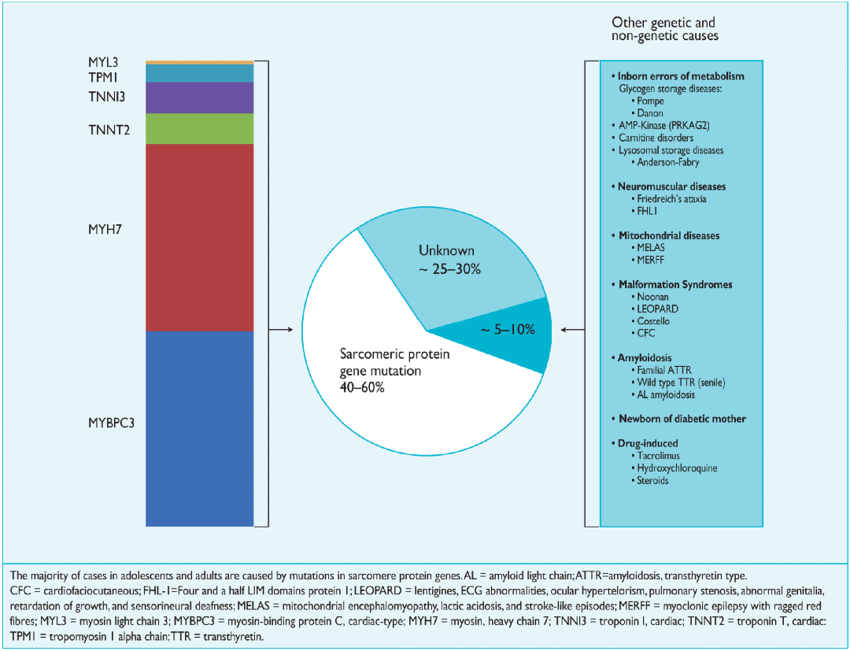 Fig-HCM2. Familial Hypertrophic Cardiomyopathy and Non-Familial
Hypertrophic Cardiomyopathy
Fig-HCM2. Familial Hypertrophic Cardiomyopathy and Non-Familial
Hypertrophic Cardiomyopathy (Akhtar, Mohammed & Elliott, Perry. (2018). The genetics of hypertrophic cardiomyopathy. Global Cardiology Science and Practice. 2018. 10.21542/gcsp.2018.36.)
Diagnosis
Since more than 50% of people suffering from HCM are patients of
Familial HCM. So, it is highly suggested that if you have any family
record related to HCM consult an expert in the field of genetic
disorders of the heart. Even though it is not a genetic issue, if you
have any of the above-mentioned symptoms consult an expert.
For the diagnosis of HCM, experts usually follow the diagnosis as:
- 1. Physical exam and medical history:
- It is a general step mostly undertaken to understand the case better and an overly critical process to understand the genetic inheritance of mutations.
- 2. Cardiac MRI:
- Through cardiac MRI left ventricle is studied for morphological evidence i.e.; left ventricular hypertrophy is detected through it.
- 3. Coronary angiography:
- The blood vessels related to heart are all studies through these tests to find out any kind of blockage in vessels that could otherwise be the cause of such symptoms.
- 4. Echocardiogram (echo):
- In this procedure ultrasound waves are used to take pictures of the heart. It helps evaluate the thickness of the heart muscle and heart’s pumping ability. Transthoracic echocardiograms are useful as well.
- 5. Electrocardiogram (ECG):
- ECG is amongst the main and most crucial tests run. This test records the electrical impulses in the heart and can detect any abnormality in the heart rate or rhythm. Ambulatory ECG should be performed for 24 hours to 48 hours (about 2 days) in patients of HCM for risk assessment.
- 6. Electrophysiology study:
- A thin tube is inserted through a blood vessel and into the heart to measure electrical activity. In simple words, it is used to locate the origin of arrythmias.
- 7. Holter monitor or Stress test:
- Both these are used to keep tract of heartbeat and its rhythm during daily life activities.
Treatment Available for HCM
Treatment strategies are based upon clinical experience and medical observations since no large, randomized trial has been performed. Pharmacological therapy is the first-line approach to treat HCM. The classes of drugs being used are categorized as:
- 1. Beta Blockers:
- Beta blockers help by slowing the heart rate and reducing the force of contraction. This, in turn, alleviates symptoms and decreases the oxygen demand on the myocardium.
- 2. Calcium Channel Blockers:
- By inhibiting calcium entry into cells, calcium channel blockers induce vasodilation and reduce the workload on the heart, contributing to symptom relief.
- 3. Antiarrhythmics:
- Antiarrhythmic medications are used to manage and prevent abnormal heart rhythms, which can be a concern in hypertrophic cardiomyopathy.
- 4. Diuretics:
- Diuretics increase urine production, helping to manage fluid retention and associated symptoms like edema and shortness of breath.
- 5. Angiotensin-Converting Enzyme (ACE) Inhibitors:
- ACE inhibitors lower blood pressure, reduce afterload on the heart, and may improve symptoms associated with hypertrophic cardiomyopathy.
- 6. Angiotensin II Receptor Blockers (ARBs):
- ARBs, similar to ACE inhibitors, contribute to vasodilation and decreased afterload, thereby helping manage symptoms.
- 7. Cardiac Glycosides:
- Cardiac glycosides, like digoxin, increase the force of cardiac contractions. In some cases, they may be used to improve symptoms and enhance pumping efficiency.
- 8. Anticoagulants:
- Anticoagulants, such as warfarin or direct oral anticoagulants (DOACs), are prescribed to prevent blood clot formation, reducing the risk of stroke in patients with hypertrophic cardiomyopathy.